| Spermatic cord | |
|---|---|
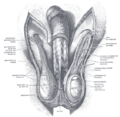
 The spermatic cord in the inguinal canal (label for spermatic cord in lower right) | |
| Details | |
| Artery | Testicular artery |
| Vein | Pampiniform plexus |
| Identifiers | |
| Latin | funiculus spermaticus |
| MeSH | D013085 |
| TA98 | A09.3.04.001 |
| TA2 | 3615 |
| FMA | 19937 |
| Anatomical terminology | |
The spermatic cord is the cord-like structure in males formed by the vas deferens (ductus deferens) and surrounding tissue that runs from the deep inguinal ring down to each testicle. Its serosal covering, the tunica vaginalis, is an extension of the peritoneum that passes through the transversalis fascia. Each testicle develops in the lower thoracic and upper lumbar region and migrates into the scrotum. During its descent it carries along with it the vas deferens, its vessels, nerves etc. There is one on each side.
Structure
[edit]The spermatic cord is ensheathed in three layers of tissue:
- external spermatic fascia, an extension of the innominate fascia that overlies the aponeurosis of the external oblique muscle.[1]
- cremasteric muscle and fascia, formed from a continuation of the internal oblique muscle and its fascia.[1]
- internal spermatic fascia, continuous with the transversalis fascia.[1]
The normal diameter of the spermatic cord is about 16 mm (range 11 to 22 mm).[2] It is located behind the tunica vaginalis.[3]
Contents
[edit]Blood vessels
[edit]Nerves
[edit]- Nerve to cremaster (genital branch of the genitofemoral nerve).
- Testicular nerves (sympathetic nerves).
The ilioinguinal nerve is not actually located inside the spermatic cord, but runs outside it in the inguinal canal.
Other contents
[edit]The tunica vaginalis is located in front of the spermatic cord, outside it.[3]
Clinical significance
[edit]The spermatic cord is sensitive to torsion, in which the testicle rotates within its sac and blocks its own blood supply. Testicular torsion may result in irreversible damage to the testicle within hours. A collection of serous fluid in the spermatic cord is named 'funiculocele'.
The contents of the abdominal cavity may protrude into the inguinal canal, producing an indirect inguinal hernia
Varicose veins of the spermatic cord are referred to as varicocele. Though often asymptomatic, about one in four people with varicocele have negatively affected fertility.[4]
Additional images
[edit]-
The left femoral triangle
-
The scrotum
-
The right testis, exposed by laying open the tunica vaginalis
-
Spermatic cord
-
Spermatic cord
-
Superficial veins oflower limb. Superficial dissection. Anterior view.
References
[edit]- ^ a b c d e f g h i Liu, Longfei (2019). "Chapter 1 - Applied Anatomy of the Scrotum and its Contents". Scrotoscopic Surgery. Academic Press. pp. 1–8. doi:10.1016/B978-0-12-815008-5.00001-7. ISBN 978-0-12-815008-5. S2CID 81721236.
- ^ Firoozabadi R, Stafford P, Routt M (2015). "Risk of Spermatic Cord Injury During Anterior Pelvic Ring and Acetabular Surgery: An Anatomical Study". Arch Bone Jt Surg. 3 (4): 269–73. PMC 4628634. PMID 26550592.
- ^ a b Yin, Zhuo; Meng, Xianxi (2019). "Chapter 4 - General Techniques of Scrotoscopic Surgery". Scrotoscopic Surgery. Academic Press. pp. 23–53. doi:10.1016/B978-0-12-815008-5.00004-2. ISBN 978-0-12-815008-5. S2CID 81292862.
- ^ "Learn About Varicocele Treatment". VARICOCELE HEALING. Archived from the original on 2 February 2014. Retrieved 25 April 2018.
External links
[edit]- Cross section image: pembody/body18b—Plastination Laboratory at the Medical University of Vienna
- Cross section image: pelvis/pelvis-e12-15—Plastination Laboratory at the Medical University of Vienna
- inguinalregion at The Anatomy Lesson by Wesley Norman (Georgetown University) (spermaticcord)